Anatomical reminder
Carpal tunnel syndrome is linked to compression of the median nerve in the wrist.
The carpal tunnel is a narrow tunnel formed posteriorly by the carpal bones and anteriorly by the anterior annular carpal ligament.
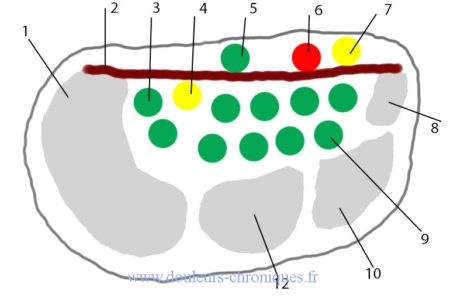
1- Trapezius bone
2- Annular ligament of the carpus
3- Tendon of the superficial flexors of the fingers
4- Median nerve
5- Palmaris longus tendon
6- Ulnar artery
7- Ulnar nerve
8- Hooked bone
9- Tendon of the deep digital flexors
10- Large bone
12- Trapezoid bone
The median nerve is a sensorimotor nerve. The sensitive territory of the nerve:
The median nerve is the motor for the abductor brevis, the flexor brevis, the opponens pollicis and the first two lumbricals.
The muscular branches of the median nerve innervate the flexor muscles of the anterior compartment of the forearm: the palmaris longus, the flexor carpi radialis, the flexor digitorum superficialis, the flexor pollicis longus, as well as the lateral half of the flexor depth of the fingers and pronator teres.
Description of carpal tunnel syndrome
It is the most common canal syndrome (80,000 interventions per year in France). It affects 4 women for 1 man.
Pain
The pain is characteristically located on the palmar surface of the first 3 fingers, but can affect the entire hand and radiate retrogradely towards the forearm and sometimes even the shoulder. They are often described as tingling, tingling, and their resurgence at night, waking the patient, sometimes calmed by waving the hand or letting it hang outside the bed. Vasomotor disorders are common with edema and excessive sweating. Initially clearly predominantly nocturnal, these disorders become, over time, diurnal, handicapping professional or domestic activities. The involvement is frequently bilateral from the outset, but always predominates on one side.
The clinical examination
The clinical examination may initially be normal; no motor or sensory deficit (Stage I). The existence of objective sensory disorders in the territory of the median nerve (50% of cases) corresponds to Stage II.
Motor disorders (deficit of the opposite thumb in 30%) are characteristic of stage III. They can be associated with amyotrophy of the thenar eminence (20%), more exceptionally with trophic lesions.
Maneuvers reproducing sensory disorders must be systematically carried out:
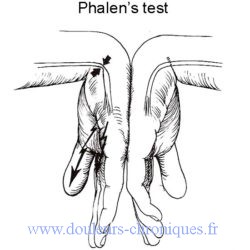
- The PHALEN forced wrist flexion test
- Percussion of the anterior surface of the wrist which awakens paresthesias or TINEL sign.
- The motor assessment focuses on the function of the thenar muscles (clamp testing)
Paraclinical examinations
Electromyogram
Highlights a lengthening of distal motor and sensory latencies with normal elbow-wrist conduction speed.
Ultrasound, CT scan and MRI are of no use in classic forms of carpal tunnel syndrome
They will be useful in the search for certain secondary forms.
It should be noted that WAGNER described the kinetics of the Median Nerve. Normally, when flexing the wrist with a closed fist, the Flexors pass above the Median Nerve which is attached to the deep plane. However, in Carpal Tunnel Syndrome, the Median Nerve remains immobile during the kinetic test, probably because it adheres to the superficial plane.
The 4 stages of WAGNER
– Normal kinetics = stage 0: the Median Nerve slides easily between the tendons of the superficial flexors of the 1st and 2nd fingers or the 2nd and 3rd fingers and is found between the 1st row and the 2nd row of flexors. There it is protected from conflict with the carpal ligament
– Stage 1: the Median Nerve remains on the surface, until a strong contraction of the Flexor tendons is caused, allowing the passage of the Median Nerve into depth.
– Stage 2: the passage is difficult or brutal with the feeling of a jump that is sometimes audible.
– Stage 3: the Median Nerve remains immobile on the surface.
Facilitating factors
The sport
The sports most affected are those that require movements and posture with grip (strong thumb-index grip, prolonged static, intense, sustained, repeated, rapid), wrist twisting, vibration absorption, cold conditions) . We find there:
- Martial arts and boxing
- Golf
- Tennis
- The archery
- Baseball
- Cycling, motorcycling, car driving
- CrossFit
Work
Work involving repeated and/or habitual wrist extension movements, hand gripping movements, prolonged pressure on the carpal or heel of the hand, repeated vibrations of the hand, for example:
- Building works
- Cashier, secretary
- Hairdresser
Pathologies
- Pregnancy
- Diabetes
- Hypothyroidism
- Menopause
- After-effects of trauma (wrist fracture for example)
- Rheumatoid arthritis, gout, autoimmune diseases
- Amyloidosis
- Morphological abnormalities (arterial, tendinous course, narrowed canal)
The treatment
Treatment of the cause if there is one (diabetes for example)
Non-drug treatments
- Wearing a removable wrist immobilization splint, to be worn mainly at night, generally for a period of 3 months. It helps keep the wrist in a neutral position to relieve symptoms.
- Osteopathic treatment by decompression and manipulation of the median nerve at the level of the carpal tunnel but also along its entire route from the cervical to the hand
- Reduction of repetitive gestures aggravating the syndrome, correction of posture disorders, particularly at work.
Drug treatments
- Level 1 analgesics (Paracetamol, NSAIDs)
- Physiotherapy, osteopathy (certain techniques are very effective in helping to release the nerve)
- Treatment of neuropathic pain in advanced forms
- Carpal tunnel infiltration with corticosteroids (no more than 2 or 3 times)
Surgical treatment
Description
It consists of relieving the compression of the nerve by a section of the retinaculum (transverse carpal ligament. It is done either by open surgery or by endoscopic surgery.
Recovery occurs in a few months.
If intervention is too late, painful after-effects, sensitivity disorders and loss of muscle strength may persist.
Complications
- CRPS type 1
- Scar neuropathy
- Persistence during the healing phase of an attachment of the nerve to the fibrosis of the surgical path with an attachment of it in the fibrosis which causes a recurrence of the carpal tunnel syndrome. This phenomenon can be demonstrated on MRI, or with dynamic ultrasound. In this specific case, re-intervention can improve the situation.
- Direct injury to the median nerve during the procedure with variable functional and painful sequelae, see type 2 CRPS