A new concept: Cicatricial neuropathy.
The most misunderstood and yet the most frequent of the neuropathies responsible for neuropathic pain.
Indeed, a recent study carried out by a Parisian pain center finds an incidence between 2.5% and 5% of operated patients.
They therefore affect around 500,000 people a year in France (1).
It is related to a trauma, a wound or a surgical intervention.
It gives variable pictures, from a simple gene to a persistent handicap.
Characteristic :
- Appears in the months following trauma, surgery.
- The pain is accompanied by dysaesthesia, paresthesia, burning, electric shocks sometimes sensation of bone pain.
- Clinical examination finds hyperesthesia and/or hypoesthesia in the area.
- Depending on the area affected, an accompanying myofascial syndrome is not uncommon.
- Complementary examinations are normal (blood test, X-ray, ultrasound, scanner, MRI)
- Only the bone scan is sometimes positive but has no value in this context.
- Electromyogram and evoked potentials are normal.
- The size of the surgery or trauma does not prejudge the size of the painful area and its consequences.
- May be responsible for visceral symptoms depending on the location of the skin lesion: constipation, bladder instability.
Diagnostic :
- The diagnosis is only clinical.
- The local examination of the patient finds the neurological signs described above.
- The territory affected may correspond to a known but often truncated neurological path (absence of complete involvement of the territory: truncated sciatica, truncated intercostal neuralgia) or be divided into “oil stains”.
- In the painful area there is a scar, even minimal (trocar path for example)
- Examination of the scarred area by the rolling palpation method triggers a sharp pain which sometimes reproduces all the pain described by the patient.
- Can join the neurological picture of vasomotor signs and sometimes edema realizing true algodystrophy (CRPS)
An algorithm to help diagnose these pains is available in the part of the site reserved for doctors.
Treatment and diagnosis confirmation:
- Infiltration of the scarred area with 1% lidocaine confirms the diagnosis. This infiltration is done by tracing infiltration under the scar and sometimes deeper in the subcutaneous plane
Short kiss needles can be used (particularly in the abdomen), which allow you to clearly feel the areas containing fibrosis and the changes in tissue density. - The injection, if the scar is responsible, is painful or even very painful, which is a good diagnostic sign.
- If the scar is not responsible, the injection is not very painful.
- In the minutes that follow, the pain associated with this scar disappears and confirms the diagnosis.
- To get an idea of the neurological picture of some patients, we invite you to look at the clinical cases described on this site.
If effective, the injection must be repeated if the pain has disappeared over a fairly long period (1,2,3 weeks or even several months). Repeated injections allow two-thirds of patients to obtain a clear improvement over the long term (2). Sometimes a single injection may be enough. - If the injection is effective but only 2 hours, it was made close to the responsible area and it is the release of lidocaine that causes relief.Do not forget to treat an associated myofascial syndrome with physiotherapy.
Action mechanism :
- Cicatricial neuropathy probably corresponds to damage to small nerves sheathed in the fibrosis of the scar.
- The latter evolves by contracting and hardening, realizing in a few weeks or months a real compression of these small nerves, which explains the delay between surgery or trauma and the appearance of these pains.
- Lidocaine infiltration probably has a mechanical effect by dissecting this fibrosis and relieving the compression of these small nerves.
- The anesthetic also probably defuses central phenomena related to this permanent pain.This mechanism of action has yet to be confirmed.
Frequency:
This notion of cicatricial neuropathy is very important to integrate because of its frequency in chronic pain. In the remainder of this article, we reviewed the records of 500 consecutive new patients treated at the pain consultation. This list was made a posteriori from June 2019 to November 2020.
The average age of patients is 52 +/- 16 years with an average age of 51.4 +/- 16 years in men and 53.2 +/- 17 years in women.
In this series of 500 patients, we find a proportion of 69% women.
We sorted the patients by painful areas and looked for the presence in this area of a cicatricial neuropathy as described in this article. The result is surprising, in fact, 48% of patients in this series present this pathology in relation to the reason for consultation.
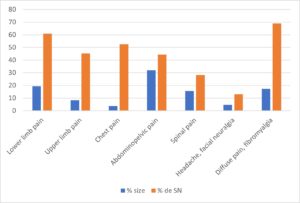
Table 1. Distribution of the different painful areas in the series and percentage of scar or cicatricial neuropathy (CN or SN) per area.