Ulnar canal syndrome at the elbow
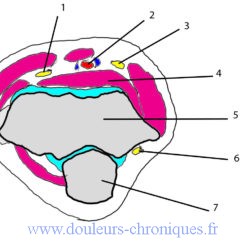
Anatomical reminder
1- Radial nerve
2- vessels
3-Median nerve
4- Brachialis muscle
5- Humerus
6-Ulnar nerve
7- Olecranon
The ulnar nerve travels in the epitrochleo-olecranon groove on the inner side of the elbow. It relates to:
- Outside the olecranon
- Medially to the epitrochleo-olecranon band (vertical band on the left diagram)
- Anteriorly to the medial epicondyle.
After this passage, it insinuates itself between the 2 heads of the flexor carpi ulnaris muscle, passing under the arch of the anterior or epitrochlear head.
The sensory territory of the ulnar nerve is located (see diagrams):
The muscles innervated by the ulnar are:
- Flexor carpi ulnaris muscle
- Fourth and fifth head of the flexor digitorum profundus muscle
- Palmar interosseous muscles
- Dorsal interosseous muscles
- Third and fourth lumbrical muscles
- Opponent muscle of the little finger
- Little finger abductor muscle
- Flexor digitorum brevis muscle
- Deep head of the flexor pollicis brevis muscle
- Adductor pollicis muscle
- Palmaris brevis muscle
Description of the syndrome
Clinical
3 clinical stages are described:
- Stage 1: paresthesias in the sensitive area of the nerve associated with pain sometimes going up to the elbow. Paresthesias and pain are increased by activity, pressing the elbow on a hard surface.
- Stage 2: appearance of hypoesthesia associated with moderate muscle damage (muscles mentioned above).
- Stage 3: severe sensory and motor impairment with appearance of amyotrophy. The pathology can lead to an ulnar claw hand (hyperextension of P1 and flexion of P2 and P3 of the 4th and 5th fingers).
On clinical examination, local impasto can be found; a Tinel sign is often found.
Paraclinical examinations
- A morphological examination of the elbow is carried out to look for a local cause (radiography and/or ultrasound and/or MRI)
- An electromyogram will confirm the conduction block at the elbow.
Etiology
Traumatic
- Direct contusion
- Elbow fracture and dislocation
- Prolonged support (bed rest, coma)
- Extended tourniquet
- Vicious callus
- Cubitus valgus (sequences of poorly corrected elbow trauma in childhood)
Secondary
Extrinsic compressions
- Synovial proliferations in rheumatoid arthritis
- Paget’s disease
- Osteophytes
- Synovial cyst
- Osteochondromatosis
Increasing the volume of content
- Nerve or soft tissue tumors
Primitives
- Background: renal failure, chronic alcoholism, diabetes
- Athletic:
- Gymnastic
- Shot put
- Tennis, baseball
- Musician:
- Violin
- Guitar
- Professional activity: work involving repeated or forced elbow flexion movements or work with prolonged support on the posterior surface of the elbow
- Painter, carpenter, joiner, plumber
- Truck driver
- Watchmaker, jeweler
- Switchboard operator
- Mechanic
- Locksmith
Treatment
- Medical treatment in beginner forms with anti-inflammatories and analgesics, night splint of the extended elbow, physiotherapy (nerve sliding exercises)
- Corticosteroid infiltrations may be proposed
- In severe forms, surgery is the only solution:
- Section of the epitrochleo-olecranon strip
- Section of the anterior ulnar arch
- Sometimes transposition of the nerve in front of the epitrochlea