The myofascial syndrome: introduction
These pains of muscular origin are encountered daily by doctors but are unfortunately poorly understood or ignored. However, they are responsible in some patients for major and disabling functional impairment.
The International Committee of Anatomical Nomenclature of Bern references 200 pairs of muscles in the human body. Each of these muscles can develop myofascial syndrome and be responsible for pain referred away from the muscle. That is to say the number of different pains of possible muscular origin.
Each muscle can have areas called trigger points or trigger points. These trigger points cause distant pain that has no neurological distribution. Trigger point pressure can trigger referred pain
Two American physicians, Dr. TRAVELL and Dr. SIMONS, have studied these syndromes for many years and written a reference book on the subject. The descriptions of myofascial syndromes are partly inspired by their work. The site will be incremented little by little with new descriptions, starting with the most frequently encountered in clinical practice.
Description of trigger points
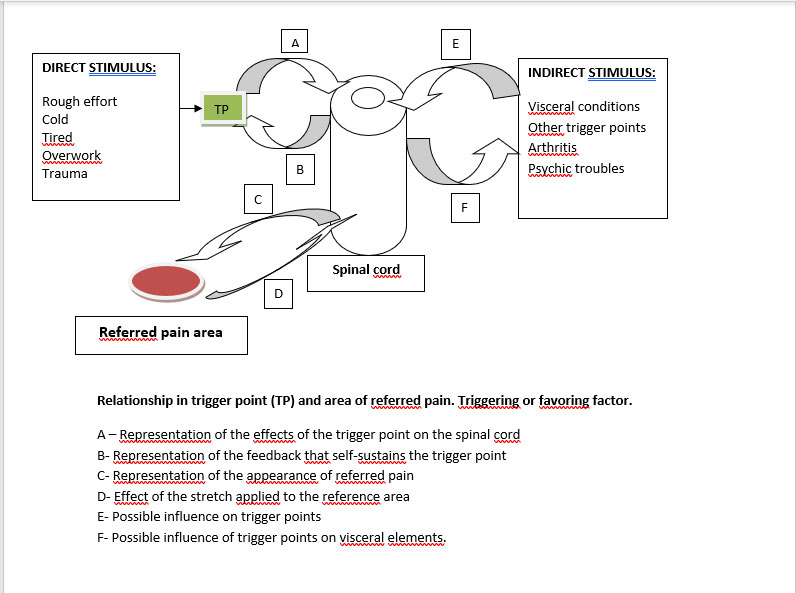
- The myofascial pain of the trigger points is projected according to characteristic and reproducible reference zones of each muscle. It uses the notion of medullary convergence.
The referred or projected pain of myofascial syndromes is, in principle, dull and persistent. Its intensity ranges from simple discomfort to unbearable pain. It can appear at rest or simply during movement of the offending part. The pain described is not on a segmental route or a usual neurological route but it is located in a part of the dermatome corresponding to the myotome of the responsible muscle. The painful surface is often variable according to the painful intensity (the simple gene is often smaller in surface than the intolerable gene). This rule is often slightly modified because the notion of medullary convergence takes on its full value without this type of phenomenon.
In this diagram the supraspinal controls do not appear but probably play a variable role during the chronicization of the painful phenomena.
- Trigger points can be activated by other trigger points, visceral damage, inflammatory joint or tendon damage, psychological disorders (it should be noted, therefore, that the participation of the brain is, as in all chronic pain , possibly) .
- Trigger points readily develop in synergistic muscles of the first muscle affected (cascade damage). Sometimes the treatment of the initial trigger point makes it possible to treat all the affected muscles.
- The pain varies in intensity and over time (depending on the activity or not, physical activity, mental state), often the pain is more intense at the end of the day than in the morning, which is not a rule.
- The level of excitability of trigger points is multifactorial. The frozen position of the muscle in the shortened position, for example during sleep, exposure to cold, a viral or bacterial infection, a stretching maneuver of an antagonist muscle, psychological stress are factors in the appearance of referred pain .
- Trigger points often persist despite the disappearance of the initial lesion. The muscle has “learned” to avoid pain. This results in chronic muscle pain. The persistence of this muscle damage over time and despite repeated treatments can lead to true muscular dystrophy.
- Neurovegetative signs can be associated with a trigger point such as:
- vasomotor disorders
- sweating disorders
- salivation disorders, lacrimation
- Dizziness, tinnitus
- Proprioception disorders are also possible
- Muscle stiffness, especially in the morning, and muscle weakness are also common
Clinical diagnosis
- In the presence of a trigger point in a muscle, its passive or active stretching causes pain. The induced muscle spasm prevents any further stretching of the muscle. As a result, there is a stretch limitation of the muscle.
- The pain is greatly increased when the muscle contracts against a fixed resistance, especially when the latter is in the shortened position.
- The contractile force of a muscle containing a trigger point is reduced.
- Paresthesias and hyperesthesia are present in the referred trigger point areas.
- Associated neurovegetative disorders are also possible (description above)
- On palpation, the muscle is tense and indurations are palpable in the trigger point area. The patient sometimes describes swellings (like lumps) in the responsible area.
These indurations disappear immediately in case of effective treatment. - During palpation, the trigger point is an area where the pain is maximal. If this point is pressed, a “muscle jump” is usual (pressing causes the patient to jump and cry).
Moderate pressure maintained on a trigger point leads to the appearance of related referred pain. - In certain locations, such as the back, the skin may present with dermographism and panniculosis or cellulo-teno-myalgia syndrome (the rolling palpation test of the skin is painful)
Myofascial syndrome. Processing
- Physiotherapy including manual techniques with deep massage (ischemic compression) followed by stretching.
- Stretching can be improved by applying cold (cryotherapy) or heat beforehand.
- Sometimes lidocaine injections into the trigger point(s) by your doctor can provide rapid improvement if followed by the same stretches.
- The K tape (sticky tape in light tension on the skin) allows these trigger points to be deactivated for a more or less prolonged period.
- A new technique is currently available, dry needling (literally “dry needle”) consisting of inserting an acupuncture needle into the contracted area (a technique in vogue in Anglo-Saxon countries and in Switzerland, under development in France).
- Whatever the techniques, we will actively seek posture disorders through an assessment of this same posture (oculomotricity, temporomandibular joint, static pelvis, podiatric study) which must be corrected in the event of an anomaly.
- The management of psychological problems, stress, anxiety are sometimes necessary for successful treatment.
- Some punctual pain relief techniques probably allow a more central rehabilitation of the painful problem during the mobilization of the affected area (ktape for example).
Muscle strengthening has also shown its effectiveness in the treatment of these pains associated with stretching (Mata Diz JB, de Souza JRLM, Leopoldino AAO, Oliveira VC (2016) Exercise, in particular the combined exercise of stretching and strengthening, reduces myofascial pain: a systematic review. Journal of Physical Therapy 63: 17-22)