Pathophysiology of neuralgia of the pudendal nerve
Classic pudendal nerve neuralgia is a tunnel syndrome (like carpal tunnel syndrome). There are two areas of possible conflict in the pelvic area:
- at the level of the ischial spine, between the sacrospinous ligament and the sacrotuberous ligament
- at the level of the canal of Alcock, splitting of the aponeurosis of the obturator muscle.
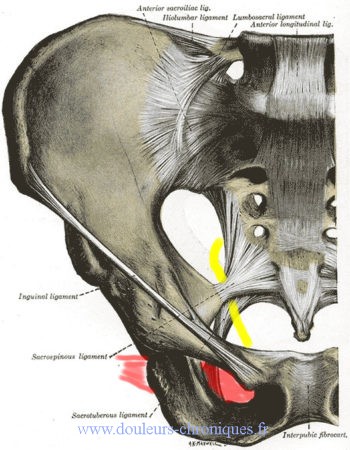
In yellow the pudendal nerve,
In red the obturator internus muscle
Symptoms of Pudendal Neuralgia
According to : Puget, B Kastler, S Aubry, L Laborie, B Fergane, E Delabrousse, Z Boulahdour, B Parratte, « Infiltration scanno-guidée en deux sites dans la névralgie pudendale », Journal de Radiologie, vol. 90, no 5 Part 1, , p. 577–582
From the most frequent to the rarest described in this article, the symptoms experienced are:
- Anal, perineal, labial, clitoris/penis, inguinal, urethral burning sensation
- Intra-rectal foreign body sensation
- Sensation of false defecation urges
- Deep dyspareunia
- Erectile dysfunction
- Pain during ejaculation
- Pollakiuria (frequent urination)
- Dysuria (difficulty urinating)
- Constipation
- Ischial pain
- Hyperesthesia, dysesthesia +/- diffuse
- Feeling of narrowing, contraction, spasm, twisting, anal, rectal or pelvic tearing
- Spontaneous sexual hyperexcitability syndrome
- Sensation of pelvic heaviness.
Diagnostic criteria for neuralgia of the pudendal nerve
They are based in particular on the Nantes criteria (2006, Labat JJ, Riant T, Robert R (Federal center for functional pelviperineal pathologies CHU Nantes), Amarenco G, Lefaucheur JP). These criteria are commented on and improved according to various observations.
Five criteria are considered essential for diagnosis
and must therefore all be present to speak of tunnel syndrome of the pudendal nerve or pudendal neuralgia
of compressive origin.
1. Pain located in the territory of the pudendal nerve (from the anus to the penis or clitoris.
As it is a truncal pain, it must be located in the territory of the nerve
pudendal which goes from the anus to the clitoris or the penis.
It can be superficial or a little deeper at the anorectal level, at the vulvovaginal level and at the level of the distal urethra.
As it is a truncal pain, it must be located in the territory of the nerve
pudendal which goes from the anus to the clitoris or the penis.
It can be superficial or a little deeper at the anorectal level, at the vulvovaginal level and at the level of the distal urethra.
This excludes pain that is exclusively localized to the coccygeal region, the sacrum, the buttocks, the pubis and the hypogastric region, but the pain may radiate to these areas.
2. Predominant pain when sitting
This is an essential clinical feature.
All nerves must be mobile so as not to be constrained during movement (example of the ulnar nerve at the elbow) or during pressure when seated for the pudendal nerve. Any loss of mobility of the nerve (where it is) will therefore expose it to crashing into rigid ligamentous structures such as the falciform extension of the sacrospinous ligament. It is indeed the hyperpressure which is
responsible and not the sitting position, which is perfectly demonstrated by the relief of the
pain on a toilet seat (provided the patient remains on it long enough).
This dynamic element is essential because if pain were linked solely to a phenomenon of
compression the pain would be continuous (which does not prevent pain from tumor lesion
which can exist standing or at night in decubitus, to be also aggravated in a seated position).
This is an essential clinical feature.
All nerves must be mobile so as not to be constrained during movement (example of the ulnar nerve at the elbow) or during pressure when seated for the pudendal nerve. Any loss of mobility of the nerve (where it is) will therefore expose it to crashing into rigid ligamentous structures such as the falciform extension of the sacrospinous ligament. It is indeed the hyperpressure which is
responsible and not the sitting position, which is perfectly demonstrated by the relief of the
pain on a toilet seat (provided the patient remains on it long enough).
This dynamic element is essential because if pain were linked solely to a phenomenon of
compression the pain would be continuous (which does not prevent pain from tumor lesion
which can exist standing or at night in decubitus, to be also aggravated in a seated position).
Very often this positional factor is exclusive but over time the pain tends to
become much more continuous even if it will always remain predominant in a seated position
3. Pain not waking up at night
This is the direct consequence of the previous criterion. Many patients may suffer in the evening, in the supine position, with difficulty falling asleep but they are not awakened by perineal pain of root canal origin. They can be awakened by accompanying symptoms (e.g. need to urinate) but not pain perineum itself. Nocturnal awakenings in the hyperalgesic phases are exceptionally found in the clinical history of patients, transiently.
4. Absence of objective sensory deficit
In the face of any perineal superficial sensory deficit, it will be necessary to evoke above all a sacral root lesion (particularly cauda equina), or sacral plexus. These proximal damage is often expressed less by pain than by deficits, loss of sensitivity or sphincter motor disorders in particular. Several explanations can be put forward for this absence of objective sensory disturbance. Lesion may be insufficient to cause significant loss of sensory fibers
superficial, as in sciatica, or in many carpal tunnel syndromes. The absence of objective sensory deficit is also based on the anatomy data, because the perineal sensitivity corresponds to the overlapping of several nerve trunks.
However, pain of scarring origin can be added to the Nantes criteria, which can lead to sensory disturbances of the whole nerve with a peripheral origin without truncal damage, and pain of muscular origin of the pelvic floor which can lead to similar symptoms.
5. Positive pudendal nerve diagnostic block (subject to flawless technique)
The realization of an anesthetic infiltration of the pudendal nerve must make the pain disappear significantly during the time of the local anesthesia. This is an essential criterion but it is not specific to the syndrome. In fact, in the event of damage to the nerve below the anesthetic block, this criterion will be validated (especially in the case of more peripheral damage, in particular scarring).
In practice, infiltration of the pudendal nerve(s) (right and left) with local anesthesia 2 to 3 ml of 1% lidocaine and a corticosteroid such as Hydrocortancyl(prednisolone) or betamethasone will be proposed. Indeed the local anesthesia makes it possible to carry out the diagnostic test and in the event of effectiveness the corticosteroids possibly makes it possible to make the treatment.
The level and side to be tested depend on the symptomatology. In case of unilateral or clearly asymmetrical symptoms, the affected side will be tested first at the ischial spine. If there is no lateralization, both sides at the level of the ischial spine will be tested.
If the local anesthesia test works but the relief only lasts two hours, a new infiltration with the same products will be performed in the Alcock canal.
Note, during these infiltrations, one can note an increase in pain in the hours following the infiltration (increase in pressure in a closed space)
Additional diagnostic criteria
Eight criteria are considered suggestive or compatible with the diagnosis of pain related to a pudendal entrapment syndrome, without however being required or specific to the diagnostic.
1. Sensations of burning, electric shocks, tightness,
numbness
Pudendal neuralgia has the characteristics of neuropathic pain. The feelings of burning, electric shocks, pulling or squeezing, numbness are part of the criteria for neuropathic pain even if more than 4 criteria are rarely found at DN4 (scale comprising 10 criteria including presence of 4 of them are necessary for the diagnosis of neuropathic pain).
2. Allodynia or hyperpathia
Allodynia and hyperpathia are highly suggestive of neuropathic involvement and are expressed at the perineal level by an intolerance to wearing tight clothing, briefs (preferring underpants to underpants), or vulvar contact (as in vestibulodynia) with superficial dyspareunia.
3. Endocavitary foreign body sensation (“symthalgia” rectally or vaginally)
Words used by patients who have deep pain, usually at the level
anorectal, sometimes at the vaginal or even urethral level, are generally quite vivid. The term of
“foreign body” is the most frequently used, other expressions are evocative:
sensation of stake, ball, heaviness, tennis ball, animal gnawing or
“grouille”… This clinical expression is sometimes called in an abusive way: syndrome of
levator, without there being any correlation with the finding of hypertonia of the levators of the anus.
These pains have a vegetative connotation and their temporary disappearance after a block
anesthetic of the sympathetic fibers at the level of the Impar ganglion evokes a mediation
by the sympathetic fibers and therefore the fact that it is “symthalgia”.
4. Worsening of pain during the day
The absence of pain in the morning upon waking, the low level of pain in the morning,
the aggravation during the day and the maximum recruitment of pain in the evening until
falling asleep is a very characteristic temporal profile of the entrapment syndrome of the nerve
pudendal.
5. Predominantly unilateral pain
Perineal pain will be all the more suggestive of pudendal truncal involvement
that it will be unilateral (and that it will be extended to the entire hemi-perineum from front to
back), but the median, central character of the pain does not in any way eliminate the diagnosis.
6. Pain appearing after defecation
One of the characteristics of pudendal pain of predominantly ductal origin
posterior is the delayed onset of pain after defecation (usually a quarter
an hour to an hour later).
7. Presence of exquisite pain on pressure of the sciatic spine
During rectal or vaginal examination, palpation of the sciatic spine (backward and a little
laterally) is very often sensitive. This is not a true sign of Tinel in the extent that this pressure does not trigger pain or paresthesias radiating down the nerve path. Moreover, this sign is not specific and can be observed outside of any
nerve compression. In fact, there are many anatomical structures at this level (passage of the pudendal nerve at the level of the sacrospinous ligament, ligamentous insertions of the ligament sacrospinatus, ischio-coccygeal bundles of the elevators) and it is very difficult to interpret this pressure pain, which may also correspond to diffuse hypersensitivity. That being, a pain caused by the pressure at this level will have all the more value as it
will be unilateral.
8. EMG (electromyogram) data in the man or nulliparous woman
Childbirth is the most common cause of perineal stretch neuropathy, which removes any specificity from the EMG examination when it is carried out in the multiparous. In on the other hand, the existence of EMG abnormalities, in particular lateralized, in men or women nulliparous may have etiological diagnostic significance, especially in the absence of an history of constipation, previous pelvic surgery or proximal lesions known, myelo-radicular or plexic.
Exclusion criteria for neuralgia of the pudendal nerve
Four criteria make it possible to exclude the diagnosis of pain related to a syndrome
pudendal canal.
1. Pain only in the coccygeal, buttocks, pubis or
hypogastric
This type of pain cannot be linked to a pudendal tunnel syndrome, because these territories
anatomical do not correspond to that of the pudendal nerve.
2. Pruritus
Pruritus above all evokes a dermatological lesion (sclero-atrophic lichen, etc.) and
not neurological pain. The notion of pruritus, which includes a need for scratching, is
distinguish from the term “itching”, which may be used by patients and which is a
DN4 neuropathic pain criterion.
3. Only paroxysmal pain
The paroxysmal, flashing pains have a neuropathic tone and could
evoke a compressive attack, but they correspond in fact a priori to the existence of a
nerve tumor. This requires exploration by imaging of the pelvic region (neurofibroma
or pudendal nerve schwannoma), cauda equina (sacral schwannoma) and spinal cord
(meningioma).
Moreover, fleeting proctalgia is sufficiently evocative not to mention it.
confused with pudendal neuralgia. However, they remain largely unknown. It is
pain that can last from a few minutes to an hour, predominantly anorectal,
mostly nocturnal, recurrent with seizures that may occur for years
several times a year, without scalability. Although some authors have been able to evoke an etiology
neurological, they are in the vast majority of cases strictly idiopathic and of controversial physiopathology.
We will add to this chapter the pains occurring exclusively during the
defecation (suggesting a proctological pathology), urination (suggesting a pathology
urological), or sexual intercourse (vaginismus, vestibulitis).
4. Imaging abnormalities that may explain the pain.
No imaging examination can demonstrate pudendal nerve compression
ductal origin, but these examinations are useful to rule out other etiologies of neuralgia
pudendal. The “trap” is to discover an intercurrent pathology, the treatment of which
will in no way change the evolution of the pain syndrome. The finding of arachnoid cysts
remains a particularly difficult problem, and conventionally these cysts are considered
asymptomatic. In any case, they cannot be held responsible for a painting
typical of pudendal neuralgia. Imaging is essential as soon as the clinical picture emerges
of the criteria described in this article and will be decisive if it shows a lesional process
which can in itself explain the pain (nerve tumor in particular).
Associated signs not excluding the diagnosis
Pudendal neuralgia can be expressed in a simple way within the framework of the criteria
diagnoses detailed above, but many patients have additional symptoms,
polymorphic and confusing that it is often difficult to relate to the pudendal nerve. Even if they
may seem surprising, the various signs dealt with in this chapter do not allow
to exclude the diagnosis as shown by clinical practice and evolution under treatment.
1. Irradiation to the buttocks or to the lower limb, especially when seated
Admittedly, the gluteal or sciatic innervation is not dependent on the pudendal nerve, and a
isolated buttock pain, even occurring while seated, cannot be considered as a pudendal neuralgia. Association of perineal neuralgia with buttock pain or sciatica can however be explained by a common impingement , rather proximal , in the channel under piriform, with concomitant involvement of the pudendal nerve, the posterior cutaneous nerve of the thigh, inferior gluteal nerve or sciatic trunk. Buttock pain may be related to
trigger points or a spasm of the deep gluteal muscles: internal obturator muscle and piriformis muscle. This can occur due to reflex muscle contractures secondary to pain, due to regional myofascial syndrome, which is extremely common in this context (evidence of regional hypersensitivity) or due to a central hypersensitivity linked to convergence phenomena between S1-S2 metamers and S3. An irradiation of the pains on the internal face of the thigh can also occur and be the witness of a syndrome of the internal obturator muscle corresponding to the conflict between this muscle and the obturator nerve.
2. Suprapubic pain
It may be the witness of hypertonia of the puborectal bundle of the levators of the anus. They may be the witness of bone hypersensitivity witnessing a secondary regional complex pain syndrome (minimal algodystrophy). They can be the witness of pain related to a cicatricial neuropathy of the suprapubic region.
3.Pollakiuria and/or bladder filling pain
Pollakiuria is often associated with pudendal neuralgia. It has the characteristic of evolving intermittently, parallel to the pain, thus making it possible to relate it to the latter and not to bladder dysfunction. There are probably synaptic interconnection phenomena with inappropriate processing of the painful message, resulting in the transmission of false urges. Sometimes the patient reports urethral pain
or hypogastric aggravated by bladder filling and relieved by urination. This justifies keeping a voiding diary, if the volumes urinated are low and very constant, it is necessary to perform a cystoscopy under general anesthesia with hydro-distension in search of signs of interstitial cystitis. On the other hand, if the volumes urinated are very variable, we will evoke phenomena of bladder hypersensitivity which may be linked to
phenomena of central hypersensitivity and vegetative reflexes.
Similarly, my presence of a sensitive scar in the supra pubic region may be responsible for this symptomatology.
4.Pain appearing after ejaculation
Confusing symptom in the absence of an infectious context (absence of vesiculitis), this
Isolated symptom can in no way be suggestive of a tunnel syndrome of the pudendal nerve.
The association with pudendal neuralgia is however quite frequent and can be considered
as evidence of regional hypersensitivity.
5. Dyspareunia and/or pain after intercourse
In pudendal neuralgia, sexual intercourse is usually spaced out. The first reason is that chronic pain syndrome impairs libido. Intercourse is rarely very painful: this is the case when there is vulvar allodynia, but in general, patients report having no pain during intercourse while the pain worsens in the following hours.
6. Erection problems
The pudendal nerve, somatic nerve, is only partially involved in erection.
Classically, its sexual function is above all sensory (dorsal nerve of the penis and
dorsal clitoris), it is also involved in pre-ejaculatory hyperrigidity and in the
clonic character of ejaculation. Patients with pudendal neuralgia will complain
willingly from a feeling of penile numbness, sexual hyposensitivity or even
a decrease in stiffness. Pain medications may also have a
negative impact on erection and ejaculation.
7.Normal EMG
Electrophysiological exploration explores only the large motor fibers and a
selective impairment of small sensory fibers, as is usual in the syndromes
ducts, will therefore have no electrophysiological repercussions. Furthermore, due to the
positional nature of pain and its pathophysiological mechanisms, it is
quite possible that pudendal neuralgia is not accompanied by structural lesions
chronic pudendal nerve fibers, and therefore no EMG abnormalities.
Findings
The diagnosis of pudendal neuralgia due to ductal involvement is above all clinical. There
has no pathognomonic criteria but more or less strong orientation elements.
When the 4 essential clinical diagnostic criteria are met (pain in the
territory of the pudendal nerve, worse when sitting, not waking up at night and without
objective hypoesthesia) it is permissible to perform an anesthetic diagnostic nerve block
pudendal whose positivity will confirm these strong elements of clinical suspicion. THE
Pudendal pain is however complex and often associated with a number of
signs whose interpretation can help to better understand and better understand
in charge of the disease.
